Immune Cells Soak Up Duchenne MD Therapy Exondys 51, Prolonging Its Work, Study Reports
by |
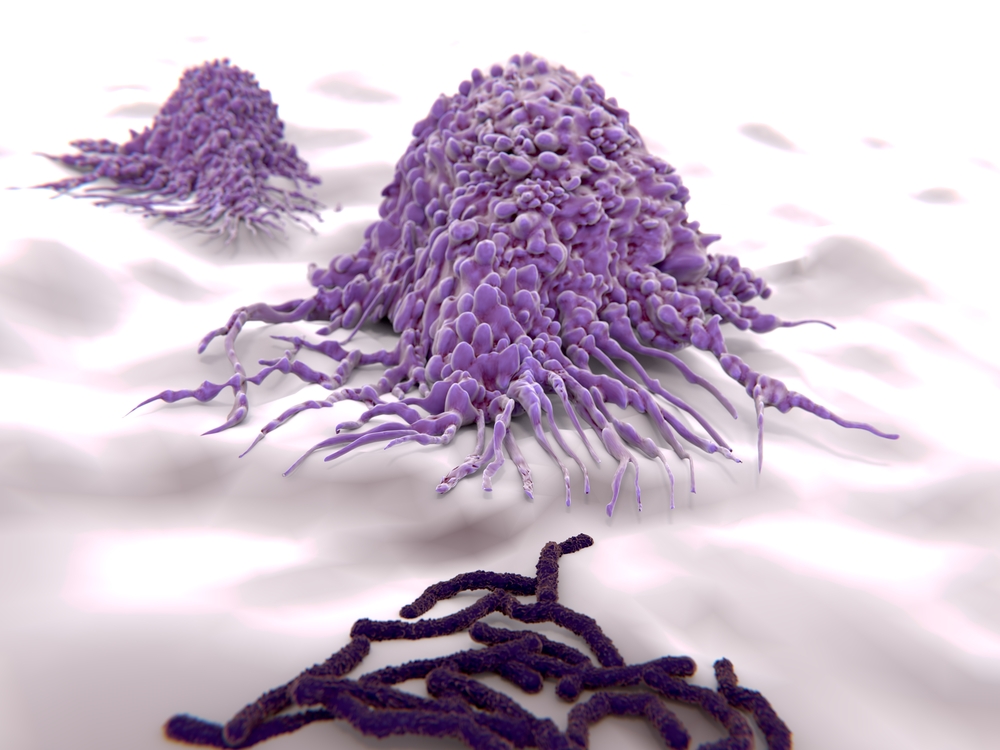
The newly approved Duchenne muscular dystrophy therapy Exondys 51 (eteplirsen) stays in immune cells several days after leaving the blood, continuing to help regenerate muscle fibers, according to a study in mice.
Researchers at the Children’s National Health System in the Washington area said the findings on immune cells known as macrophages shed light on the cell mechanisms that help deliver DMD treatments. This understanding could lead to strategies that increase the therapy’s effectiveness, they said.
The study, “Myoblasts and macrophages are required for therapeutic morpholino antisense oligonucleotide delivery to dystrophic muscle,” was published in the journal Nature Communications.
Last year Exondys 51 became the first exon-skipping treatment for DMD to obtain U.S. Food and Drug Administration approval. Sarepta Therapeutics designed the drug to correct the genetic defect underlying the disease. The idea was that fixing the abnormality would restore levels of the dystrophin protein that is missing in muscles.
Exondys 51 showed promise in preclinical-trial studies. Clinical trial results were mixed, with some patients responding well and others not so well. The FDA approved it because the trials showed that it did help some patients, however.
A possible explanation why Exondys 51 failed to help other patients was its rapid clearance from the blood – within hours. The Children’s researchers decided to investigate the mechanisms underlying the therapy’s delivery to cells. Their thought was that a better understanding of the delivery system could allow them to tweak the system, increasing the therapy’s effects.
Dr. Terence Partridge, principal investigator of the Children’s Center for Genetic Medicine Research, led the research effort. He was the study’s lead author.
The work involved a mouse model of DMD with a faulty dystrophin gene — the same situation found in humans with the disease. The researchers attached a fluorescent tag to the therapy so they could see where it went once it was inside the mice.
It ended up in the animals’ muscles — specifically in areas where muscle is regenerated. In these areas the fluorescent tag accumulated inside macrophages. Those immune cells penetrate muscles to respond to the inflammatory process that accompanies muscle regeneration.
Contrary to its fast clearance from blood, the tag remained inside macrophages up to a week. The therapy then passed to muscle stem cells, the active players in muscle regeneration.
“These macrophages appear to extend the period of availability of this medication to the satellite cells and muscle fibers at these sites,” Partridge said in a press release. “Since the macrophages are acting as long-term storage reservoirs for prolonged delivery to muscle fibers, they could possibly represent new therapeutic targets for improving the uptake and delivery of this medicine to muscle.”
The team now plans to see if they can use macrophages to deliver Exondys 51 directly to muscles, which would prevent its clearance from the blood.
“Understanding exactly how different classes of exon-skipping drugs are delivered to muscle could open entirely new possibilities for improving future therapeutics and enhancing the clinical benefit for patients,” said Dr. James S. Novak, another principal investigator at the Children’s Center for Genetic Medicine Research and the first author of the study.