Bone Health Varies Greatly Among FSHD Patients, Study Suggests
by |
Bone health varies greatly among patients with facioscapulohumeral muscular dystrophy (FSHD), according to the results of a small group study, and tests for strength and functionality may identify those with higher risks for decreased bone health.
The study “Bone Health in Facioscapulohumeral Muscular Dystrophy: A Cross-Sectional Study” was published in the journal Muscle & Nerve.
Patients with FSHD are burdened with impaired function of muscles in the face, shoulders, upper limbs, lower limbs and in the abdominal and pelvic area. This has a significant impact on patients’ quality of life, as they experience decreasing motor function, chronic fatigue and pain.
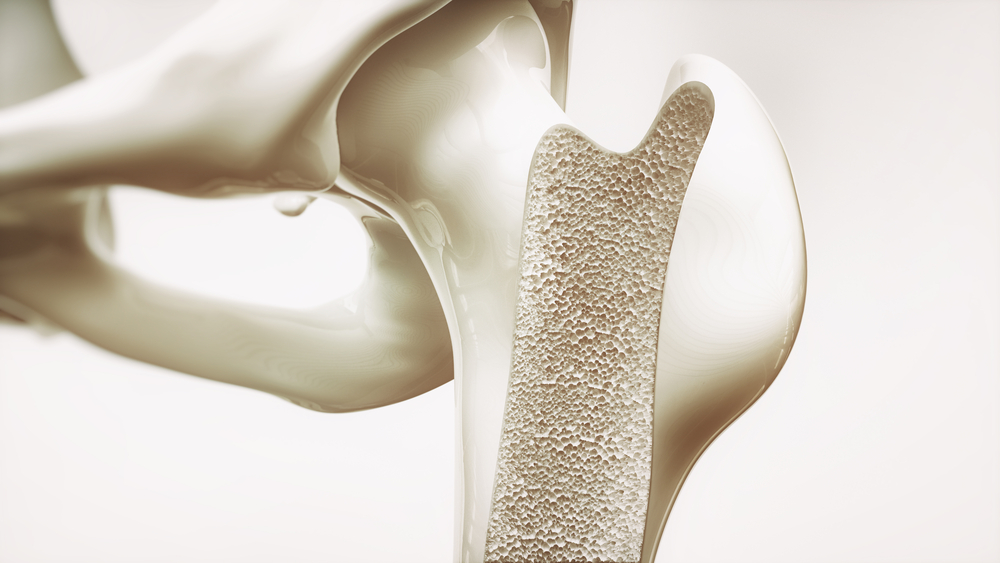
Besides muscle, bone health also is compromised in muscular dystrophies, with patients exhibiting low bone mineral density (BMD). In FSHD, however, there is a dearth of studies regarding patients’ bone health.
Authors of this study aimed “to comprehensively characterize bone health among individuals with FSHD by exploring indicators, including BMD, bone serum biomarkers, muscle strength assessments, and fracture history.”
They investigated specifically if FSHD patients show reduced BMD and whether there was a correlation between BMD levels and fractures with muscle strength or function.
To this end, authors performed a cross-sectional study, which enrolled 94 adult patients with FSHD Type 1 recruited at the Kennedy Krieger Institute in Baltimore, Md., and Concord Hospital in Concord, NSW, Australia.
The team analyzed patients’ clinical characteristics and the levels of several biomarkers of bone health, including calcium, phosphorus, 25-hydroxy vitamin D, among others. In addition, authors explored correlations between bone mineral density (BMD), strength and function.
Analysis of the 94 patients showed they presented highly variable disease severity scores, BMD, muscle strength and functionality. Researchers observed high prevalence of fractures and vitamin D3 deficiency (approximately 30% of the patients).
“However, biomarkers of bone resorption were mostly normal and did not indicate uniformly reduced bone turnover in FSHD as has been observed in Duchenne muscular dystrophy (DMD),” the study authors wrote.
Moreover, authors detected “moderately strong correlations between strength, function and whole body and regional BMD.” This suggests that tests evaluating these functions may indicate patients’ bone health status.
“Overall, given the variability in BMD and strength as well as the prevalence of fractures, effective treatment plans must be tailored based on individual BMD and strength to prevent fractures and promote optimal bone health. This may include periodic dual-energy X-ray absorptiometry scan (DXA) scans particularly in those whose strength and functional testing may predict a higher risk for impaired bone health,” the authors concluded.