New Gene Therapy to Fix Dystrophin Deficiency in DMD Shows Promise in Mice, Study Shows
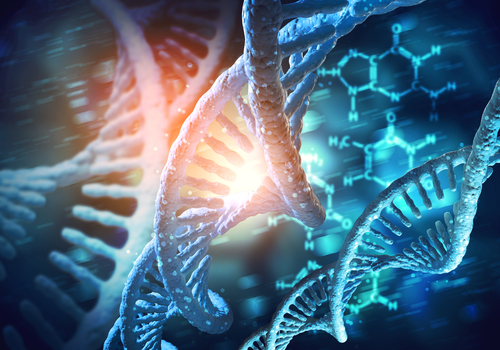
Researchers at the University of Missouri have developed a new method to efficiently deliver the correct form of dystrophin gene to muscles as a way to correct the faulty gene that characterizes Duchenne muscular dystrophy (DMD), a mouse study shows.
Their study, “A Five-Repeat Micro-Dystrophin Gene Ameliorated Dystrophic Phenotype in the Severe DBA/2J-mdx Model of Duchenne Muscular Dystrophy,” appeared in the journal Molecular Therapy—Methods & Clinical Development.
DMD is caused by a modification of the gene that encodes the dystrophin protein, which is essential for normal muscle activity. Such mutations interfere with production of the functional protein, severely affecting muscle fiber structure and strength.
Correcting the faulty gene could potentially treat this disease. Several attempts at gene therapy have been tried, but all have failed to efficiently reverse all DMD symptoms.
Gene therapy commonly uses vectors based viral genetic sequences to achieve the desired gene transfer capacity. The therapeutic potential of these techniques rely not only on the delivery system, but also on the sequence of the gene of interest that is used. In this case, smaller versions of dystrophin known as microdystrophin must be used, since its natural form is just too big to be useful in gene therapy.
“There have been other gene-transfer vectors attempted in the past (such as adenoviral vector, herpes simplex virus and plasmid), but they have largely been unsuccessful due to the complexity of the disease, challenges associated with delivery, and the large size of the native dystrophin gene,” the study’s senior author, Dongsheng Duan, said in a news release.
Duan’s team used an engineered form of the adeno-associated virus (AAV) vector to replace the damaged gene specifically in the muscles.
Researchers also used a version of the dystrophin gene that can potentially minimize the toxicity signs commonly associated with such methods, such as inadequate blood supply and fatigue during muscle contraction. This AAV viral vector has also been used in the past, but this is the first time researchers have combined it with such a version of dystrophin.
This strategy boosted levels of dystrophin protein in the muscles of mice models of DMD, and significantly reduced some disease symptoms. Yet researchers could not accurately measure the impact of this new potential therapy to correct DMD-associated effects on the hearts of the animals.
“Human studies have shown that one-time intramuscular injection of an AAV vector can result in the expression of a therapeutic protein for many years. For example, a study showed Factor IX expression for 10 years in a hemophilia patient,” Duan said. “In preclinical studies in murine and canine models, we have also observed persistent multiyear microdystrophin expression from AAV vectors. In the case of mice, a single injection can lead to microdystrophin expression throughout the lifespan.”