Discussion
Discussion
Muscular dystrophy diagnosis
Last updated Aug. 29, 2025, by Lindsey Shapiro, PhD

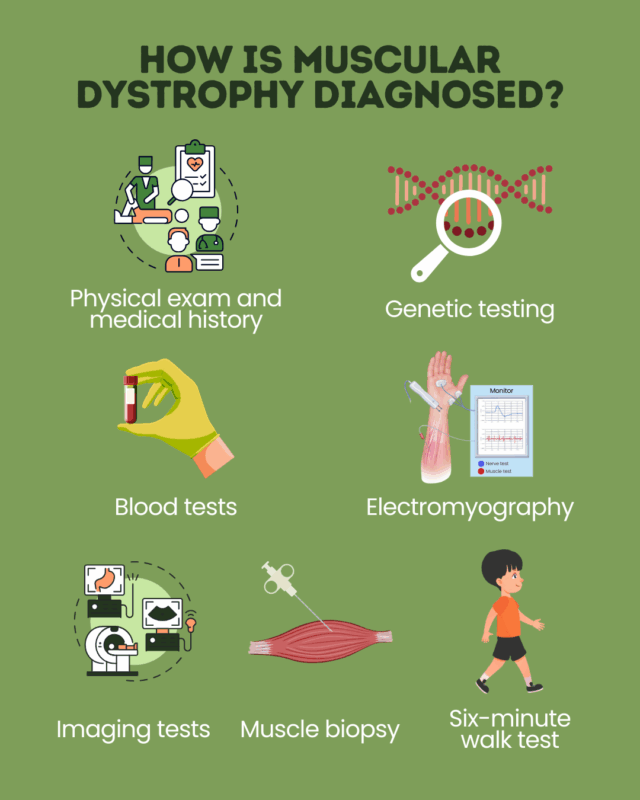
There are several tests clinicians use to diagnose muscular dystrophy (MD), a group of genetic disorders characterized by progressive muscle weakness.
An early and accurate MD diagnosis is important because it allows patients to start working with their care team on a treatment plan that will improve their long-term outlook and quality of life.
The importance of an early diagnosis
Diagnosing MD can be challenging because there are more than 30 types of MD that vary in how and when symptoms manifest. Such complexity can lead to substantial diagnostic delays.
It is important for MD to be accurately diagnosed as soon as possible. While there’s no cure for MD, initiating the right treatments early can substantially improve long-term outcomes, helping to slow disease progression and delay motor declines, ease symptoms, and improve life quality.
An early diagnosis can also help people living with the disease make informed family planning decisions, since MD is caused by genetic mutations that are often inherited within families.
How is muscular dystrophy diagnosed?
Diagnosing MD begins with a thorough clinical evaluation during which a physician will collect the patient’s medical history and perform a physical exam to look for warning signs such as:
- a family history of MD or another muscular disorder
- if a person has been experiencing MD symptoms in their daily life, such as motor function delays or frequent falls
- signs of muscle weakness, low muscle tone, or weak reflexes
- abnormal spine curvature, or scoliosis
- joint stiffness
Symptom patterns can provide clues as to the MD type. For example, a Duchenne muscular dystrophy diagnosis may be suspected when a child has MD early signs like motor delays, a history of frequent falls, and difficulty rising from the floor.
If MD or another muscular disorder is suspected, a series of other MD tests will confirm a diagnosis. If they haven’t already, a person may at this point be referred to a neuromuscular specialist who has expertise in conditions that affect muscle function.
Genetic testing
Genetic testing is the most definitive MD diagnosis test. A small sample of tissue or bodily fluid — often saliva or blood — is analyzed to look for the genetic mutations that are the underlying causes of MD. Genetic testing for MD can be done when a person has active symptoms or has a family history that puts them at risk for carrying a mutation.
In addition to diagnosing MD, genetic testing helps identify the MD type, since each is caused by mutations in different genes. The specific type of mutation in the affected gene also determines a person’s eligibility for mutation-specific treatment approaches or clinical trial participation.
Families may be referred for genetic counseling before and after their genetic testing to help them prepare for and understand their test results.
Blood tests
Blood tests to look for markers of muscle damage, particularly creatine kinase levels, are often among the first tests that are run when MD is suspected.
Creatine kinase, as well as aldolase and myoglobin, are commonly elevated in people with MD, especially in earlier disease stages.
However, these markers are not specific to the disease; rather, they simply provide evidence that muscle damage is occurring. As such, blood tests for MD can support, but can’t alone establish a diagnosis.
Electromyography
EMG, or electromyography, for MD is done to assess the health of muscles and the nerves that control them (motor neurons). It helps to determine whether the problem that’s causing muscle weakness is coming from the nerves or muscles.
With an EMG, a tiny needle electrode is inserted directly into a muscle to record its electrical activity at rest and in response to stimulation. A nerve conduction study, which measures the electrical signals coming from motor neurons via electrodes placed over the skin, is usually done at the same time.
The pattern of abnormalities in these tests can help physicians diagnose MD and rule out other neuromuscular disorders that mimic it. In people with MD, the muscle won’t respond as well to stimulation as it normally should, but nerve conduction may be mostly normal.
Imaging tests
Imaging tests such as MRI and ultrasound that visualize the muscles and tissues surrounding them can aid in diagnosing MD and monitoring its progression.
In MD, muscle tissue degenerates and is often replaced by fat tissue over time, which can be observed in an MRI for MD. Other characteristic signs of muscle damage and inflammation can also be seen on imaging tests. The specific pattern of damage may help doctors determine the MD type.
Muscle biopsy
A muscle biopsy is a diagnostic approach in which a small sample of muscle tissue is collected and examined under a microscope to look for cellular changes characteristic of MD and to rule out other disorders. The sample is often collected with a needle or small skin incision.
This test is not done as commonly as it used to be now that genetic testing can definitively establish the disease. But in rare cases where genetic testing doesn’t find a mutation and MD is still suspected, a doctor may recommend a muscle biopsy for MD.
Six-minute walk test
The six-minute walk test (6MWT) is a standard clinical evaluation that assesses a person’s physical function by testing how far they can walk on a flat, hard surface within six minutes.
While not used to firmly establish an MD diagnosis, a 6MWT can help assess endurance and exercise capacity, and is commonly used to monitor changes in function over time.
Signs to look out for
The early signs of muscle weakness in children and adults with MD may be subtle, but it’s important to recognize the symptoms that may indicate a need to have further clinical evaluation for MD. In children, this could include:
- taking longer than expected to sit up, stand, crawl, or walk
- frequent falls or clumsiness
- trouble running, jumping, or climbing stairs
- difficulty rising from a sitting or standing position, often requiring the use of hands to push off the thighs (Gowers’ sign)
- walking on tiptoes or waddling gait
- enlarged calf muscles
- speech delays
Signs that could indicate a possible MD diagnosis in adults or older children could also include:
- difficulty walking or lifting things
- muscle pain and stiffness
- joint tightness
- eyelid drooping or facial weakness
The symptoms of different forms of MD can vary. People who experience these or any other unexpected symptoms should reach out to a doctor for further evaluation, especially if they have a known family history of MD.
Next steps after diagnosis
Once an MD diagnosis is reached, it is important to work with a multidisciplinary care team to establish an individualized MD treatment and management plan. This may involve medications, physical therapy, occupational therapy, and other interventions.
Depending on the specific care needs, an MD care team could include a neuromuscular specialist, physical therapist, cardiologist, dietitian, and speech therapist.
Living with MD can be emotionally challenging. After an MD diagnosis, it’s also important for patients and families to have strategies in place that support their emotional well-being, such as counseling, therapy, or support groups.
Muscular Dystrophy News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- How AI can support my daily life with Duchenne muscular dystrophy
- Ahead of this year’s MDA Conference, association’s CEO speaks of ‘hope’
- A blind date with a book encourages me to dust off my social life
- New research reveals protein pathway that can slow muscle repair
- Dreaming of solutions to the Olympic-sized challenges of FSHD
Related articles
-
 Discussion
Discussion
-
-