Duchenne Muscular Dystrophy Patients’ Stem Cells Faulty, According To Stanford University Study
 According to a new research study by scientists at the Stanford University School of Medicine in mouse modeling of Duchenne muscular dystrophy, faulty connective-tissue genes associated with symptoms like fibrosis and muscle weakness are expressed in muscle stem cells of afflicted subjects.
According to a new research study by scientists at the Stanford University School of Medicine in mouse modeling of Duchenne muscular dystrophy, faulty connective-tissue genes associated with symptoms like fibrosis and muscle weakness are expressed in muscle stem cells of afflicted subjects.
As with human patients, mice with a particular type of Duchenne muscular dystrophy experience progressive muscle degeneration and connective tissue accumulation with increasing age. The Stanford researchers have found that the malfunction may derive at least partly in stem cells surrounding muscle fibers, and that during the disease’s course, stem cells’ ability to build new muscle are diminished and they begin expressing genes that stimulate connective tissue formation.
Excess connective tissue — or fibrosis — begins to accumulate in many bodily organs, including the vital heart, lungs, liver, and is associated with many different disorders. In people with muscular dystrophy, fibrotic tissue in skeletal muscles impairs muscle fiber function, leading to the increased muscle weakness and stiffness that are muscular dystrophy’s hallmarks.
The Stanford researchers discovered that in laboratory mice, the stem cell anomaly they’ve revealed can be inhibited by dosing the animals with a drug already approved for use in humans. The drug works by blocking a particular signaling pathway involved in fibrosis development, They caution that much more research will be required, but indications are promising, leading to hope that a similar approach will eventually be available for children battling muscular dystrophy.
 “These cells are losing their ability to produce muscle, and are beginning to look more like fibroblasts, which secrete connective tissue, says Stanford professor of neurology and neurological sciences Thomas Rando, MD, PhD, in a Stanford release. “It’s possible that if we could prevent this transition in the muscle stem cells, we could slow or ameliorate the fibrosis seen in muscular dystrophy in humans.”
“These cells are losing their ability to produce muscle, and are beginning to look more like fibroblasts, which secrete connective tissue, says Stanford professor of neurology and neurological sciences Thomas Rando, MD, PhD, in a Stanford release. “It’s possible that if we could prevent this transition in the muscle stem cells, we could slow or ameliorate the fibrosis seen in muscular dystrophy in humans.”
Dr. Rando is senior author of a paper published Dec. 17 in the journal Science Translational Medicine describing the Stanford research team’s findings. He is also director of the Glenn Laboratories for the Biology of Aging — whose focus is on the fundamental biological processes underlying the process of cellular, tissue, and organismal aging, with a particular emphasis on stem cell aging, and founding director of the Stanford Muscular Dystrophy Association Clinic. Lead author is former postdoctoral scholar Stefano Biressi, PhD, now at the Dulbecco Telethon Institute, Centre for Integrative Biology, University of Trento, Povo, Italy. The other coauthors are Elen H. Miyabara of the University of Sao Paulo’s Institute of Biomedical Sciences and the Paul F. Glenn Laboratories; and Suchitra D. Gopinath and Poppy M. M. Carlig of the Paul F. Glenn Laboratories for the Biology of Aging and Department of Neurology and Neurological Sciences, Stanford University School of Medicine
In the paper, entitled “A Wnt-TGF2 axis induces a fibrogenic program in muscle stem cells from dystrophic mice” (Sci. Transl. Med. Vol. 6, Issue 267, p. 267ra176 (2014) DOI: 10.1126/scitranslmed.3008411), the scientists report their previous observation that Wnt signaling activates a fibrogenic program in adult muscle stem cells, called satellite cells, during aging.
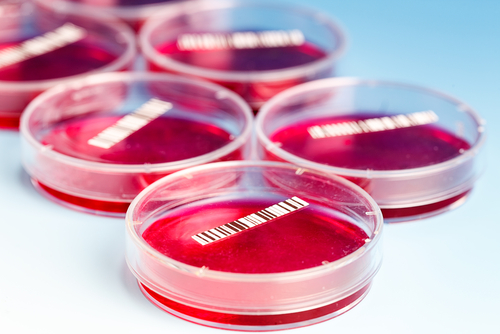
“We genetically labeled satellite cells in a mouse model of Duchenne muscular dystrophy to follow their fate during the progression of the disease,” they note, observing that a fraction of satellite cells had a reduced myogenic potential and evidenced enhanced profibrotic gene expression compared with age-matched controls.
[adrotate group=”3″]
Combining in vitro and in vivo results, the researchers observed that transforming growth factor2 (TGF2) expression was induced in response to elevated canonical Wnt signaling in dystrophic muscles, and that a resulting uptick in TGF activity affected behavior of satellite cells in an autocrine or paracrine fashion.
“Indeed,” they note, “pharmacological inhibition of the TGF pathway in vivo reduced the fibrogenic characteristics of satellite cells. These studies shed new light on the cellular and molecular mechanisms responsible for stem cell dysfunction in dystrophic muscle and may contribute to the development of more effective and specific therapeutic approaches for the prevention of muscle fibrosis.”
Duchenne muscular dystrophy afflicts roughly 1 in every 3,600 boys born in the United States, who will usually experience progressively more severe muscle weakness, which will eventually confine them to a wheelchair in early adolescence and lead eventually to full paralysis. The disorder is caused by mutated dystrophin genes, which encode the dystrophin protein whose function is to connect muscle fibers to surrounding external matrixes thereby preventing injury. Duchenne muscular dystrophy sufferers are nearly always boys because of the dystrophin genes being located on the X chromosome. A girl would need to inherit two faulty dystrophin gene copies, highly improbable because male carriers often die in early adulthood.
The researchers maintain that it’s possible that if this transition in the muscle stem cells could be prevented, it should be possible to slow the fibrosis process seen in human cases of muscular dystrophy. Under normal conditions, muscle stem cells respond to muscle damage by dividing into two cells, one of which forms the basis of new muscle growth, the other remaining a stem cell. In mice missing the dystrophin gene, the muscle stem cells gradually assume an altered state, more resemblant of fibroblasts that muscle-making factories.
For their research, Drs. Biressi and Rando used a strain of laboratory mice with muscle stem cells engineered to glow on exposure to fluorescent light when treated the drug called tamoxifen — most commonly associated with cancer treatment. The scientists bred these mice with another mouse strain in which the dystrophin gene is mutated, and monitored the fate of the cells over time.
They observed that expression of myogenic genes, that is: genes associated with muscle regeneration after an injury, was almost totally lacking in many mouse muscle stem cells after as few as 11 month,s. Meanwhile expression of defective fibrotic genes increased compared with levels in control animals. Dystrophic animals’ cells were also observed to be oddly located, Instead of being normally nestled alongside muscle fibers, they had begun to migrate into space between tissues.
The Role Of A Signaling Pathway
Drs. Rando and Biressi knew similar, but substantially less pronounced, accumulation of connective tissue in muscle fibers occurs during a normal aging process governed by signaling proteins such as the Wnt and TGF-beta protein families. THey note that Wnt plays a critical role in both embryonic development and cancer, while TGF-beta controls cell division and specialization. Consequently, they wondered whether Wnt pathway blocking in dystrophic mice would inhibit fibrosis formation in muscles.
Using the hypertension (high blood pressure) drug Losartan, which inhibits expression of TGF-beta types 1 and 2 genes, the researchers theorized that it would also probably interrupt the signaling pathway dysfunction that leads muscle stem cells astray. And indeed, Losartan did in fact prevent muscle stem cells in treated mice from expressing fibrosis-associated genes and moreover also to partially maintain their ability to form new muscle.
“This scar tissue, or fibrosis, leaves the muscle less elastic and impairs muscle function,” Dr. Rando notes in the release, “So we’d like to understand why it happens, and how to prevent it. It’s also important to limit fibrosis to increase the likelihood of success with other possible therapies, such as cell therapy or gene therapy.”
What’s Next
Because TGF-beta type 1 is a multi-role player throughout the body, the Stanford researchers are now investigating ways to specifically inhibit TGF-beta type 2 — the one involved in muscle stem cell transition, as well as in learning how their might to translate to address of other diseases.
“Fibrosis seems to occur in a vicious cycle,” Dr. Rando observes. “As the muscle stem cells become less able to regenerate new muscle, the tissue is less able to repair itself after damage. This leads to fibrosis, which then further impairs muscle formation. Understanding the biological basis of fibrosis could have a profound effect on many other diseases.”
The Stanford research was funded by the National Institutes of Health (grants AG036695, AG023806, AR062185 and AR056849), the Department of Veterans Affairs, the Muscular Dystrophy Association and the Coordenao de Aperfeioamento de Pessoal de Nivel Superior of Brazil.
Sources:
Stanford University School of Medicine
Glenn Laboratories for the Biology of Aging
Science Translational Medicine
Image Credit:
Stanford University School of Medicine