Engineered Muscle May Fix Muscle Wasting in Muscular Dystrophy
Written by |

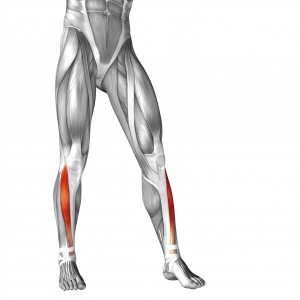 Muscle wasting in muscular dystrophy may be repairable using a new approach developed by a collaboration among researchers in Italy, Israel, and the United Kingdom. Published in EMBO Molecular Medicine, a new study, “In Vivo Generation of a Mature and Functional Artificial Skeletal Muscle,” engineered a muscle in the laboratory that could be integrated into the legs of mice who had undergone denervation or laceration of the tibialis anterior.
Muscle wasting in muscular dystrophy may be repairable using a new approach developed by a collaboration among researchers in Italy, Israel, and the United Kingdom. Published in EMBO Molecular Medicine, a new study, “In Vivo Generation of a Mature and Functional Artificial Skeletal Muscle,” engineered a muscle in the laboratory that could be integrated into the legs of mice who had undergone denervation or laceration of the tibialis anterior.
The study represents a significant step forward in both the field of muscular dystrophy research and the field of tissue engineering. Skeletal muscle is notoriously difficult to engineer due to the number of factors required for successful integration in vivo. Muscles require innervation and blood supply in order to function, which must be provided by the host tissue. “The morphology and the structural organization of the artificial organ are extremely similar to, if not indistinguishable from, a natural skeletal muscle,” stated Dr. Cesare Gargioli, principal investigator on the study, in a press release.
To allow such a seamless integration of engineered muscle into host tissue, the researchers started with mesoangioblasts (muscle precursor cells) grown on poly(ethylene glycol)-fibrinogen hydrogels. This system of cells and support matrix provided the right mix of natural and synthetic materials that could be tuned for optimal tissue properties.
[adrotate group=”3″]
Adding to this system, the mesoangioblasts used for the study were genetically transduced to produce placental-derived growth factor, which is a signaling factor that stimulates blood vessel and nerve growth in surrounding cells when the graft is implanted in the host. Upon implantation, the graft survived due to proper oxygenation and maturation of skeletal muscle fibers derived from differentiating mesangioblasts.
These grafts closely resembled normal muscle. They functioned similar to a normal tibialis anterior and were able to replace damaged muscle in the receiving mice. Noted Dr. Giulio Cossu, co-senior author on the paper, “While we are encouraged by the success of our work in growing a complete, intact, and functional mouse leg muscle, we emphasize that a mouse muscle is very small, and scaling up the process for patients may require significant additional work.” The next step is thus engineering muscle to replace the tibialis anterior in larger animal models before scaling up to human patients with muscle wasting conditions, such as muscular dystrophy, for clinical trials.





