PPMD Launches Pilot Duchenne Newborn Screening Program in NY
Written by |
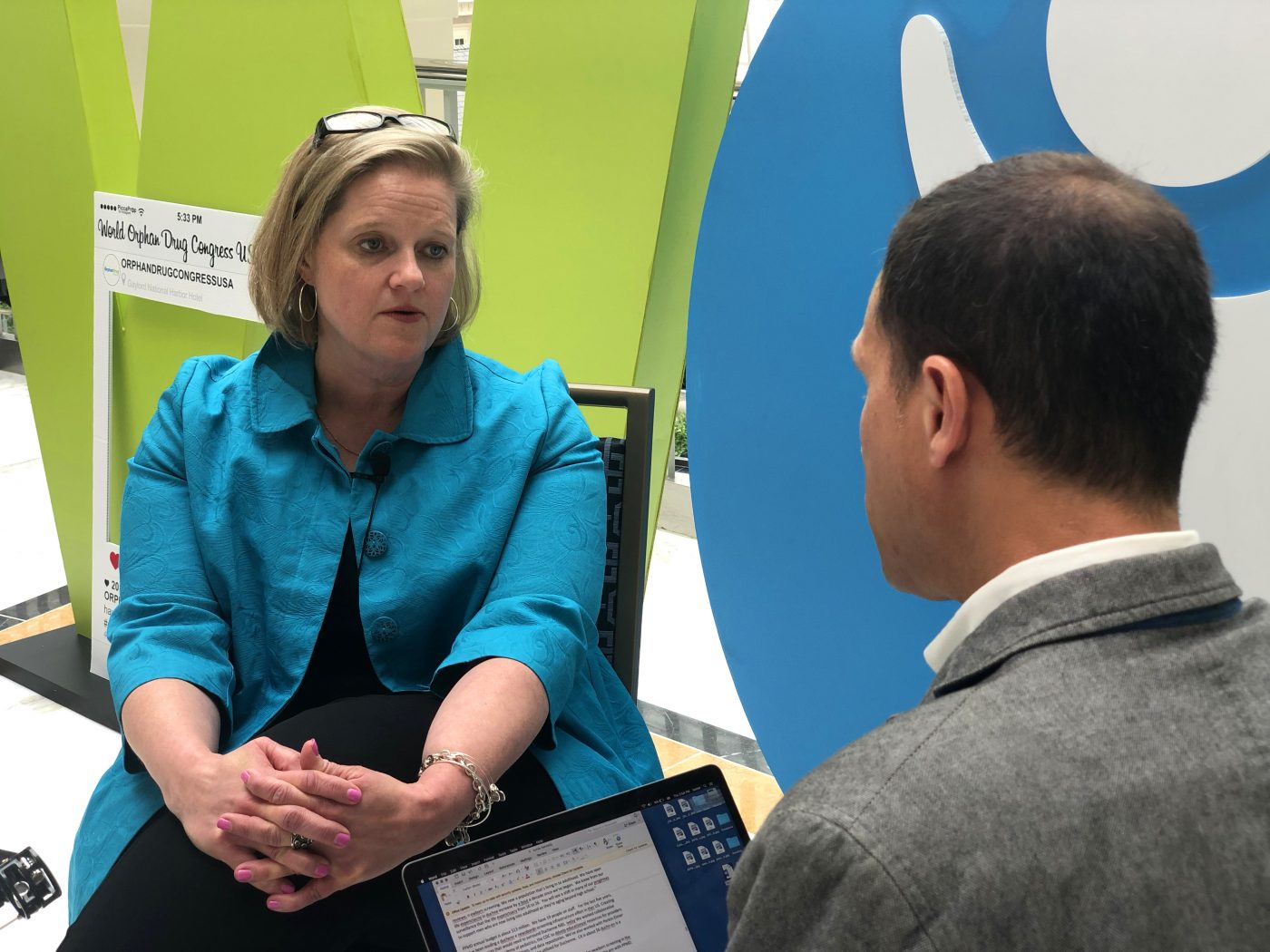
PPMD's Annie Kennedy being interviewed at the WODC 2019 conference. (Photo by Isaura de los Santos)
Parent Project Muscular Dystrophy (PPMD) has launched a pilot program to screen newborns in New York state for Duchenne — one of the most common forms of muscular dystrophy.
The $5 million program aims to screen 100,000 babies — about half of all those born each year in the Empire State — over a two-year period, said Annie Kennedy, PPMD’s senior vice president of legislation and public policy.
“The goal is that, at the end of our pilot, we will then be able to nominate Duchenne for the Recommended Universal Screening Program (RUSP),” Kennedy told Muscular Dystrophy News during the recent 2019 World Orphan Drug Congress USA. “That will have to track with our therapy development pipeline, and right now we have three gene therapies in clinical trials for Duchenne. But we couldn’t wait to start our pilot until there was an approved therapy.”
U.S. lawmakers introduced the Newborn Screening Saves Lives Reauthorization Act in the House of Representatives on May 3. The bipartisan bill — endorsed by 15 patient advocacy groups, including PPMD — provides states with the resources they need to improve their newborn screening programs and to uniformly test for all disorders on the RUSP panel.
The Newborn Screening Saves Lives act, originally approved in 2008 and renewed in 2014, must be reauthorized again by U.S. Congress.
“A simple set of tests can make a lifetime of difference,” Massachusetts Rep. Katherine Clark — vice-chair of the House Democratic Caucus and one of the bill’s four co-sponsors — said in a PPMD press release. The act, she said, “will fund essential programs and research to ensure that infants can receive effective, comprehensive screenings for treatable conditions.”
Newborn screening’s broad value
With 19.5 million inhabitants, New York ranks as the fourth most populous U.S. state (after California, Texas, and Florida). The program will be carried out by two New York City hospital networks: Northwell Health, whose affiliated hospitals together account for 17% of all births statewide, and New York-Presbyterian, with branches throughout the New York metro area.
“There’s definitely a health economic equation that goes into this,” Kennedy said. “We have to collect data to demonstrate that it’s more cost-effective to start treating babies with Duchenne earlier than when they present [with the disease] later, at age 4 or 5.
“Newborn screening does not create babies with Duchenne, it identifies them earlier. Ultimately, you will save money by treating babies earlier, because you’re ensuring optimal outcomes.”
For the last four years, she said, PPMD has been leading a national effort to build a newborn screening infrastructure for Duchenne. Taking the best practices of an Ohio pilot led by Jerry Mendell, MD, “we refined the systems further so that they could be replicated in a state with a high birth rate — and eventually nationwide.”
PPMD’s steering committee includes the American Academy of Pediatrics, the Centers for Disease Control & Prevention, Baby’s First Test, and the EveryLife Foundation for Rare Diseases. Six companies comprise the funding consortium: Sarepta Therapeutics, PTC Therapeutics, PerkinElmer, Solid Biosciences, Wave Life Sciences and Pfizer.
Decoding Duchenne
Kennedy’s organization, based in Hackensack, New Jersey, was founded in 1994 by Pat Furlong, as well as other parents and grandparents of Duchenne boys. It currently has 19 paid staffers and operates on an annual budget of $13 million.
“We have seen life expectancy in Duchenne increase by about a decade since we began,” Kennedy said. “We know from our surveillance that life expectancy has gone from 16 to 26. You will see a shift in many of our programs to support men who are now living into adulthood as they’re aging beyond high school.”
PPMD also maintains the Decode Duchenne program, which provides free genetic testing and counseling to people who would otherwise not be able to afford such testing — whose costs often run into the thousands of dollars. This includes full analysis of the Duchenne gene through next-generation sequencing, targeted testing, or repeat testing for those who need it.
PPMD added carrier testing for women one year ago; since Duchenne almost always strikes only boys, such testing is often not covered by insurance — even though “women need to know whether they’re carriers,” Kennedy said. This is also why PPMD is funding a national carrier study at Nationwide Children’s Hospital in Columbus, Ohio, that’ll ultimately enroll 400 women.
“PPMD is dedicated to fighting Duchenne and serving families from every angle,” Kennedy added. “We are the only organization focusing on legislative strategy and regulatory work. We also have comprehensive care in clinical guidelines.”
And, she continued, “we also have 26 certified Duchenne care centers, basing this on the CFF [Cystic Fibrosis Foundation] model. We now have international partners reaching out to us, wanting us to certify their care centers.”