Traditional Chinese Medicine Used to Help DMD Patients in Study
Written by |
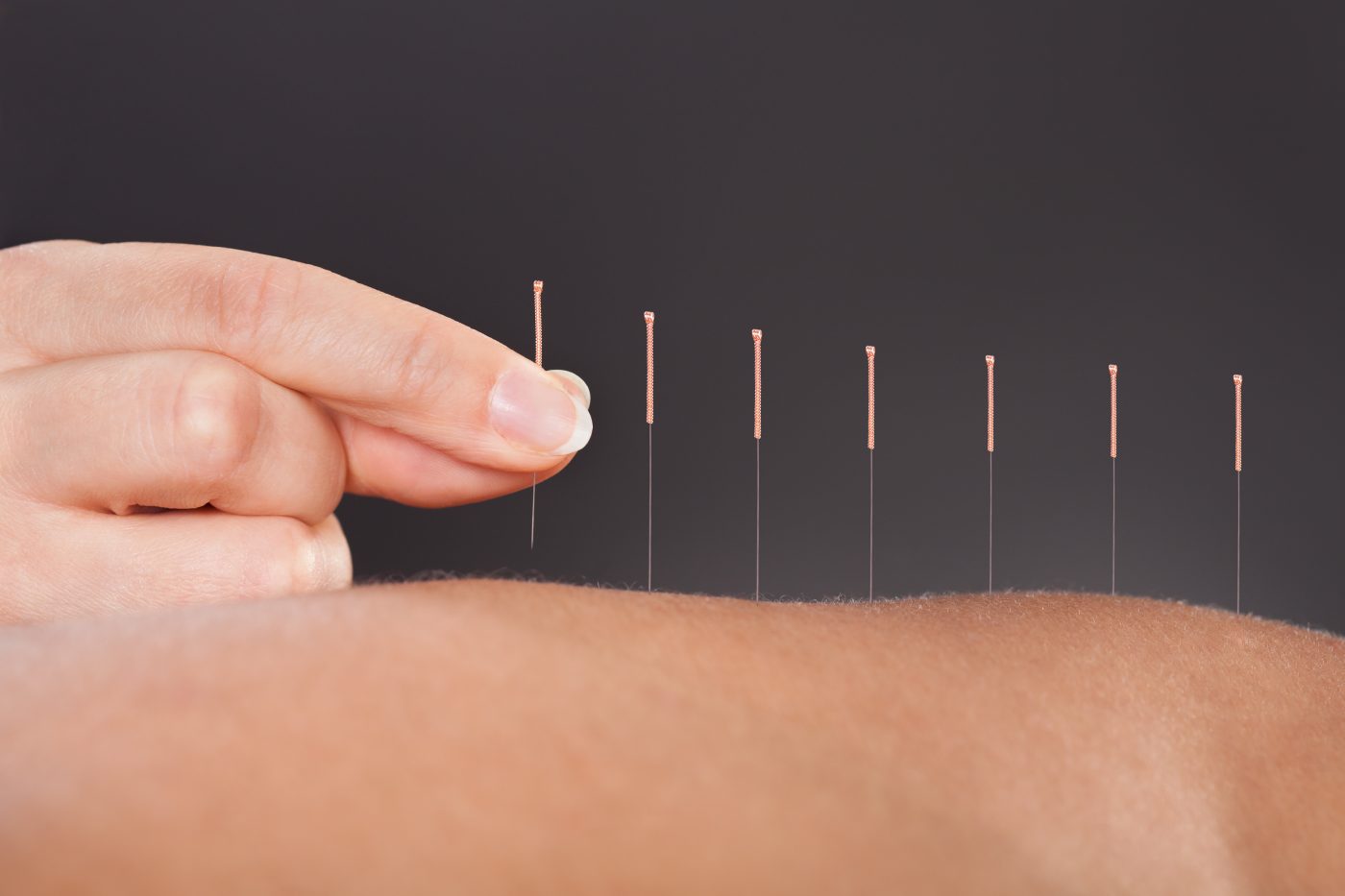
While groundbreaking discoveries rooted in the laboratory are making progress in treating children with Duchenne muscular dystrophy (DMD), acupuncture and Traditional Chinese Medicine (TCM) also hold potential to help alleviate symptoms and enhance muscle function. A team of researchers combined a number of alternative therapies along with drug therapy to create a treatment regimen for DMD patients. During the study, the regimen resulted in a significant improvement in physical function and reduced inflammation in the patients’ bodies.
The research team enrolled 60 pediatric DMD patients at the Neurology and Rehabilitation Department at Zhengzhou Children’s Hospital. Upon enrollment, patients were divided into treatment and drug-only groups. The treatment group received acupuncture, far infrared therapy, TCM tuina massage, herbal medicine, and drug therapy, while the drug-only group received drug therapy alone. Treatment lasted for a total of two years.
The so-called TCM toolkit has been expanding over the years, benefiting children with DMD. Under the practice of TCM, progressive muscular dystrophy is considered part of Wei Zheng, also known as flaccidity syndrome. Acupuncture is suggested to help DMD because TCM correlates kidney deficiency to biomedical genetic mutation disorders, and acupuncture has been used successfully for over 1,000 years to treat these concerns. Infrared heat lamp in TCM is used to enhance microcirculation, and tuina massage was included to benefit nerve and muscle fibers.
Interested in Muscular Dystrophy News research? Sign up for our forums and join the conversation!
TCM herbs were also used as the drug component of the treatment regimen. The herbs were derived from reishi mushrooms (Lingzhi) and delivered in an injectable formulation. Additional herbs and supplements included oral levocarnitine, oral fructose sodium diphosphate, and Bozhi glycopeptide injection.
Following treatment, patients saw a total effective rate improvement of 20% in the full treatment group compared to the drug-only group. Total effective improvement is calculated using full recovery, significant recovery, and effective as three parameters of improvement. The calculation led to a total effective rate improvement of 93.3% in the full treatment group and 73.3% in the drug-only group.
In addition, the full treatment group experienced significant improvements in enzymes and saw a reduction in CPK, LDH, and AST. Enhanced enzyme profiles were indicative of lower inflammation in the full treatment group when compared to the drug-only group.
Although the treatment regimen used multiple types of TCM, and each component required a protocol, incorporating TCM into a patient’s daily schedule may be useful. This treatment cohort saw significant improvements. Future tests should further support these results.





