Immunotherapy Could Improve Duchenne Muscular Dystrophy Outcomes
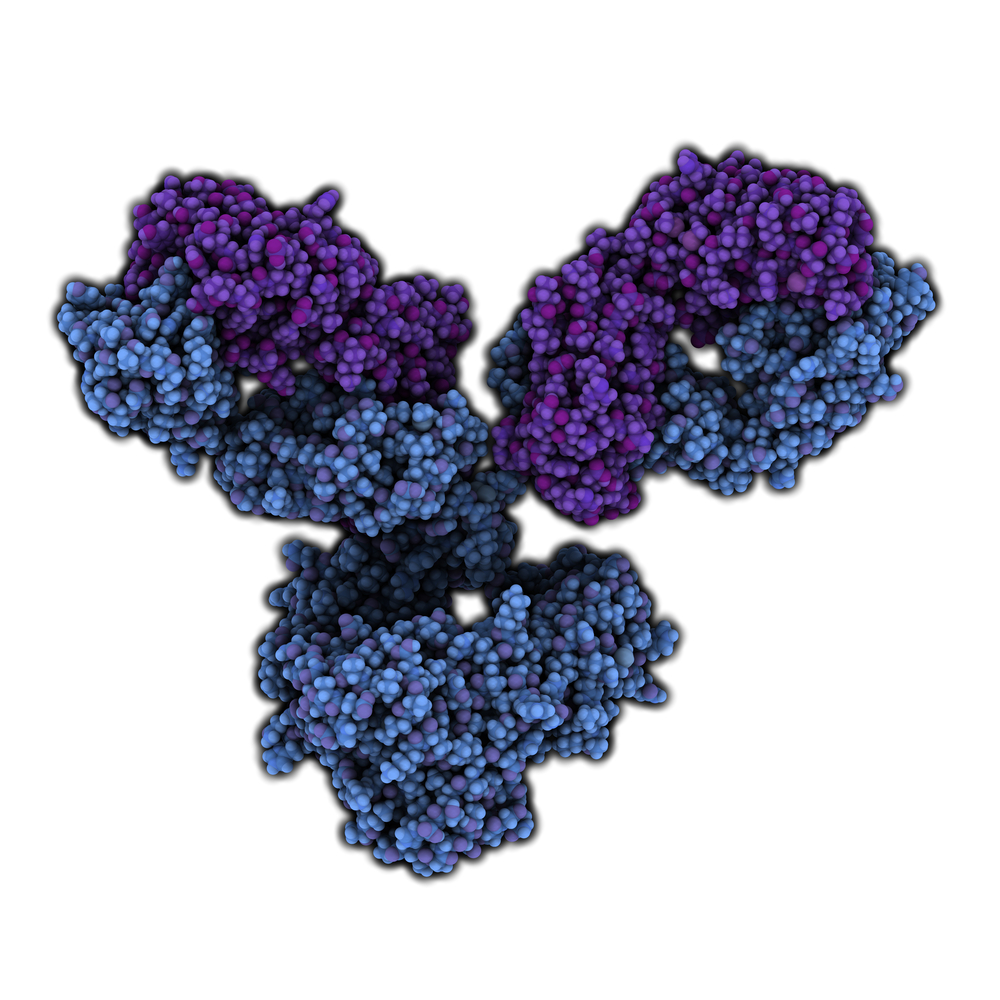
New research out of Germany indicates that immune therapy might help treat Duchenne muscular dystrophy (DMD), a serious disease that causes muscle weakness. In a mouse model of the disease, the ability to run, as well as disease biomarkers, appeared to improve following antibody treatment, specifically a form of human immunoglobulin G (IgG). The work could open the door for the development of new treatments for DMD. The article, titled “Treatment with human IgG improves the early disease course in a mouse model of Duchenne muscular dystrophy“ appeared in July 31st in the Journal of Neurochemistry.
DMD is a genetic disease in which severe muscle degeneration occurs. It usually occurs in boys, and causes a progressive loss of muscle function, beginning in the lower limbs. The DMD gene encodes the muscle protein, dystrophin. The standard treatment for DMD is the use of glucocorticosteroids, but unfortunately these drugs have many side-effects.
Led by first author Jana Zschüntzsch at the Universitätsmedizin Göttingen, Göttingen, Center for Neurological Medicine, the scientists sought to test whether an immune system therapy might be used for the treatment of the disease, by first testing what is known as an immunoglobulin G (IgG) in an experimental mouse model of DMD. They compared the IgG treatment to an injection that did not contain the treatment (control), given when the mice were both 3 and 7 weeks old.
Researchers measured the ability of the animals to run in a wheel. After 8 weeks, they also measured several biological markers in the blood, diaphragm and lower limb muscles. The IgG treatment decreased serum creatine kinase and mRNA levels of relevant inflammatory markers in the diaphragm and limb muscles. Serum creatine kinase is a DMD biomarker which indicates that an immune system process might be in overdrive. When the immune system is activated, it can be beneficial in the short term, but can be damaging over the long term. Cells that participate in the inflammatory response, known as macrophages, also went down in the quadriceps muscles due to IgG treatment.
In their report, the researchers stated that “Collectively, this study demonstrates that, in the early disease course of [DMD] mice, human IgG improves the running performance and diminishes myopathic damage and inflammation in the muscle. Therefore, IgG may be a promising approach for treatment of DMD.”
The study may be a first step in the development of new treatments for DMD, hopefully with reduced side effects relative to the current standard, glucocorticoids. Naturally scientists will need to conduct studies in humans before the promise of IgGs for DMD can be realized.






