New Tool Shows Profound Metabolic Changes in DMD Patients’ Muscles
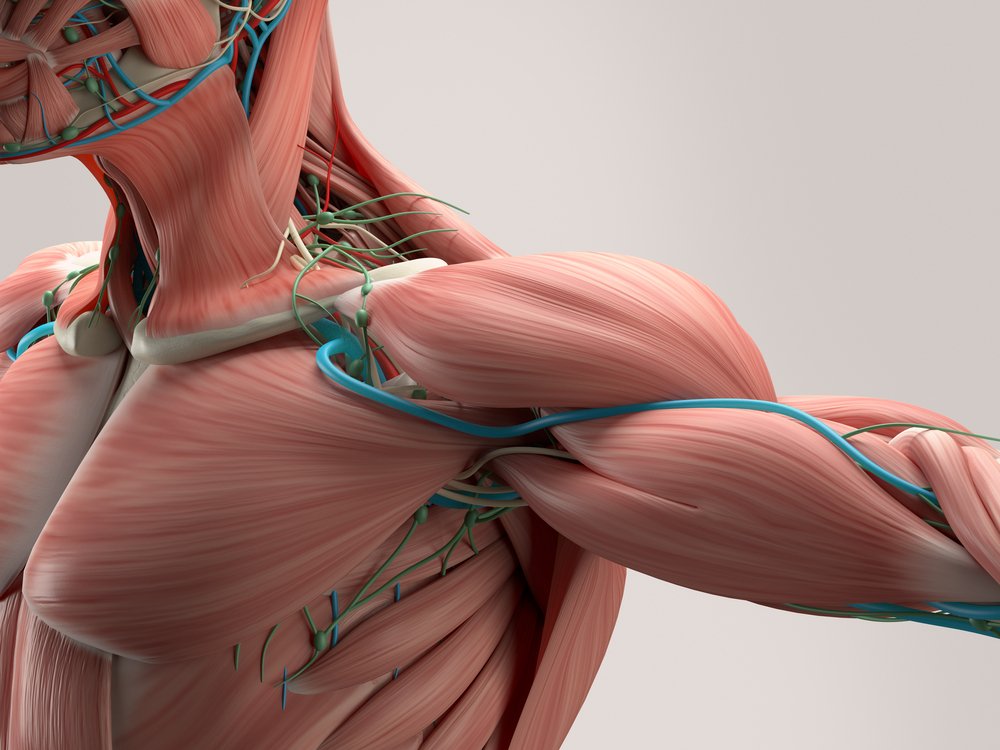
The muscles of people with Duchenne muscular dystrophy (DMD) show profound impairment, with changes in fatty molecules and energy metabolism, as compared with those of their healthy peers, a small French study revealed.
While previous studies have reported such metabolic changes in DMD patients, this was the first to analyze all metabolic molecules in a single experiment using a powerful new technique.
These and future findings using this innovative tool may help identify new therapeutic biomarkers, targets, and approaches for DMD, the researchers said.
The study, “Muscle metabolic remodelling patterns in Duchenne muscular dystrophy revealed by ultra-high-resolution mass spectrometry imaging,” was published in the journal Scientific Reports.
The protein dystrophin, critical to muscle fiber function and stability but also involved in cognitive function and brain development, is lacking in people with DMD, the most common of the more than 30 types of muscular dystrophy. As such, dystrophin deficiency leads to severe architectural changes in muscles and to muscle degeneration.
The researchers noted that “metabolic impairments have been associated with DMD since the 1970s.” But it is only now that new technology allows scientists to explore “the metabolism and its components in an unprecedented holistic and unbiased manner,” the researchers wrote.
Mass spectrometry, a technique that identifies and quantifies all molecules in a sample, has been widely used to analyze changes in metabolites, the intermediate or end products of metabolic reactions.
In addition, mass spectrometry imaging or MSI can simultaneously reveal the spatial distribution of multiple molecules in a single experiment. Knowing the spatial distribution of metabolites is “highly valuable for gaining a mechanistic understanding of biological processes,” the team wrote.
Now, researchers in France have used a new MSI-based technique — which they say provides greater resolution, sensitivity, and specificity — to compare muscle metabolic patterns between DMD patients and healthy men. Of note, sensitivity is a test’s ability to correctly diagnose a disease or its symptoms, while specificity is the ability of a test to accurately identify the absence of a disorder or its symptoms.
Altogether, the study involved 18 people: nine DMD patients with a mean age of 5.5 years at the time of muscle biopsy, and nine unaffected men, ages 28–58.
The analysis identified 34 metabolites whose levels were significantly different between muscle samples of the DMD patients and those of the healthy individuals. In all, 27 of these metabolites were found at higher levels in DMD patients’ muscles, while seven showed significantly lower levels.
The greatest differences between the groups concerned energy metabolites and phospholipids. The main fatty components of cell membranes, phospholipids also are found in the protective layers covering nerve fibers and are involved in cell signaling.
These results suggest that both metabolic pathways “are important players in muscle [damage] and possibly by extension cognitive/behavioral disabilities” in DMD, the researchers wrote.
The team noted that the findings are consistent with previous studies showing a disruption in phospholipid and energy metabolism in DMD patients.
Additionally, calcium balance — essential for energy metabolism, and muscle and nerve cell health — and the function of mitochondria, which are the powerhouses of the body’s cells, were previously shown to be altered in people with DMD.
As such, the researchers hypothesized that phospholipid changes and calcium impairment in DMD patients may promote the improper function of the mitochondria, leading to disruptions in energy metabolism.
“This study revealed a deep metabolic remodeling in phospholipids and energy metabolism in DMD,” the team wrote, adding that these findings may “open new avenues for deeper biological investigations to uncover new therapeutic targets, biomarkers and diagnostic tools.”
The results also highlighted “the potential use of MSI technology coupled with systems biology approaches to holistically explore metabolic impairments in DMD,” the researchers added.
One limitation of this study, however, is the absence of muscle samples from age-matched healthy individuals, the researchers said. They noted that the use of adult muscle samples may limit the interpretation of the results, as the biochemical properties of muscles change with age.