High Levels of Sarcolipin Protein Underlie Muscle Wasting, Cardiac Disease in DMD
Written by |
Researchers have found that lowering the the levels of a protein called sarcolipin lessens muscle weakness and improves skeletal and cardiac muscle function in a mouse model of Duchenne muscular dystrophy (DMD). These findings suggest that therapeutics targeting sarcolipin may have significant benefits to DMD patients.
The study “Reducing sarcolipin expression mitigates Duchenne muscular dystrophy and associated cardiomyopathy in mice” was published in the journal Nature Communications.
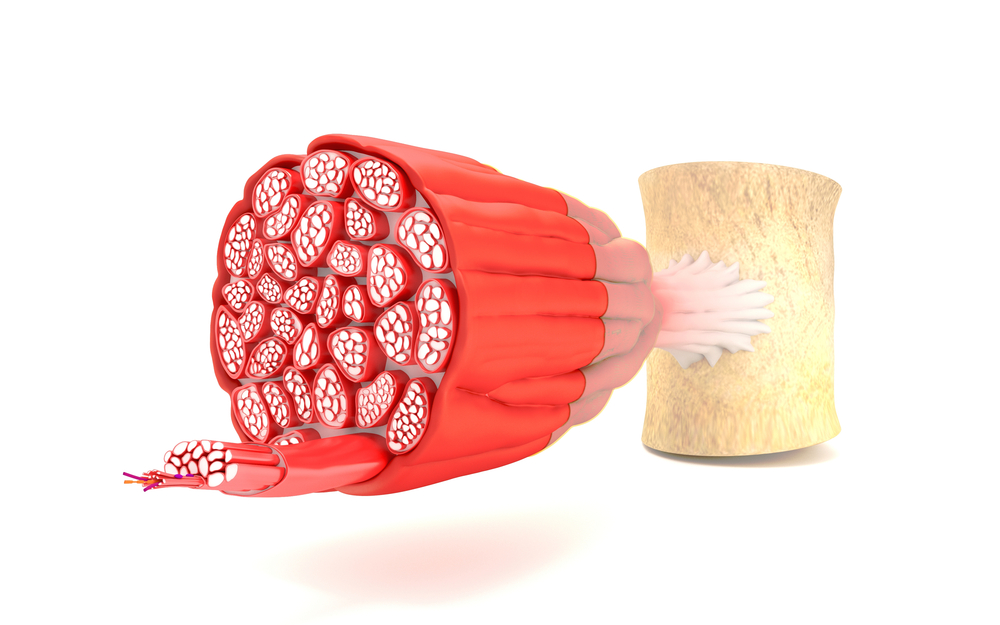
Abnormally high levels of calcium inside muscle cells increasingly are recognized as a key event that initiates and promotes DMD. One of the mechanisms leading to this calcium overload is the reduced activity of a calcium pump – the so-called sarco-endoplasmic reticulum calcium ATPase or SERCA.
Sarcolipin is an inhibitor of SERCA and researchers recently have found that the inhibitor was unusually high in cardiac and skeletal muscles of a mouse model for DMD. However, if sarcolipin increased underlying SERCA dysfunction and contributed to muscle wasting was unknown.
To understand the role of sarolipin in DMD, researchers at the Rutgers New Jersey Medical School and colleagues generated a mouse that was knocked-out (deleted) for sarcolipin and presented severe DMD.
They observed that the mice lifespan was extended upon deletion of sarcolipin compared to control mice. Also, researchers found that the high level of sarcolipin was the major contributor of SERCA dysfunction in the DMD mice muscles.
Reducing sarcolipin expression not only halted muscle degeneration, but it boosted muscle regeneration processes and improved the function of the skeletal muscles.
Additionally, “normalizing SLN [sarcolipin] level is sufficient to preserve cardiac function and mitigate dystrophic cardiomyopathy in mice,” the authors wrote.
To strengthen the potential therapeutic effect of normalizing sarcolipin expression, researchers decreased its levels in 1-month old mice. (In previous experiments mice were born without or with lower levels of sarcolipin.)
In agreement with what they already had observed, reducing sarcolipin postnatal expression mitigated severe skeletal and cardiac muscle muscular wasting.
Overall, “this study provides evidence that SLN [sarcolipin] upregulation is a molecular basis for SERCA dysfunction in both skeletal and cardiac muscles of DMD,” the authors wrote.
Most important, “we have provided initial evidence that SLN [sarcolipin] could be a common and potent therapeutic target for the treatment of diaphragm and skeletal muscle pathology and cardiomyopathy in DMD,” the study concluded.





