hiPSCs To Study And Identify Novel Drug Targets In Duchenne Muscular Dystrophy
In a new study entitled “Early pathogenesis of Duchenne muscular dystrophy modelled in patient-derived human induced pluripotent stem cells” a team of scientists developed an induced pluripotent stem cell model to study Duchenne muscular dystrophy and discover new therapeutic drugs. The study was published in the journal Scientific Reports.
Duchenne muscular dystrophy (DMD) is characterized by progressive muscle degeneration, ultimately leading to patients’ death. The disease is caused by lack of a functional dystrophin protein, an essential protein for the structural stability of muscles fibbers, including skeletal, diaphragm and heart. Various types of deletions or mutations in the dystrophin gene lead to loss of dystrophin protein expression. While some strategies have been developed to treat this devastating disease, such as exon-skipping (a sequence-specific technique) it is necessary to develop a technique that allows scientists to discover new treatments, effective in a wide range of patients, independently on the type of mutations they may harbor.
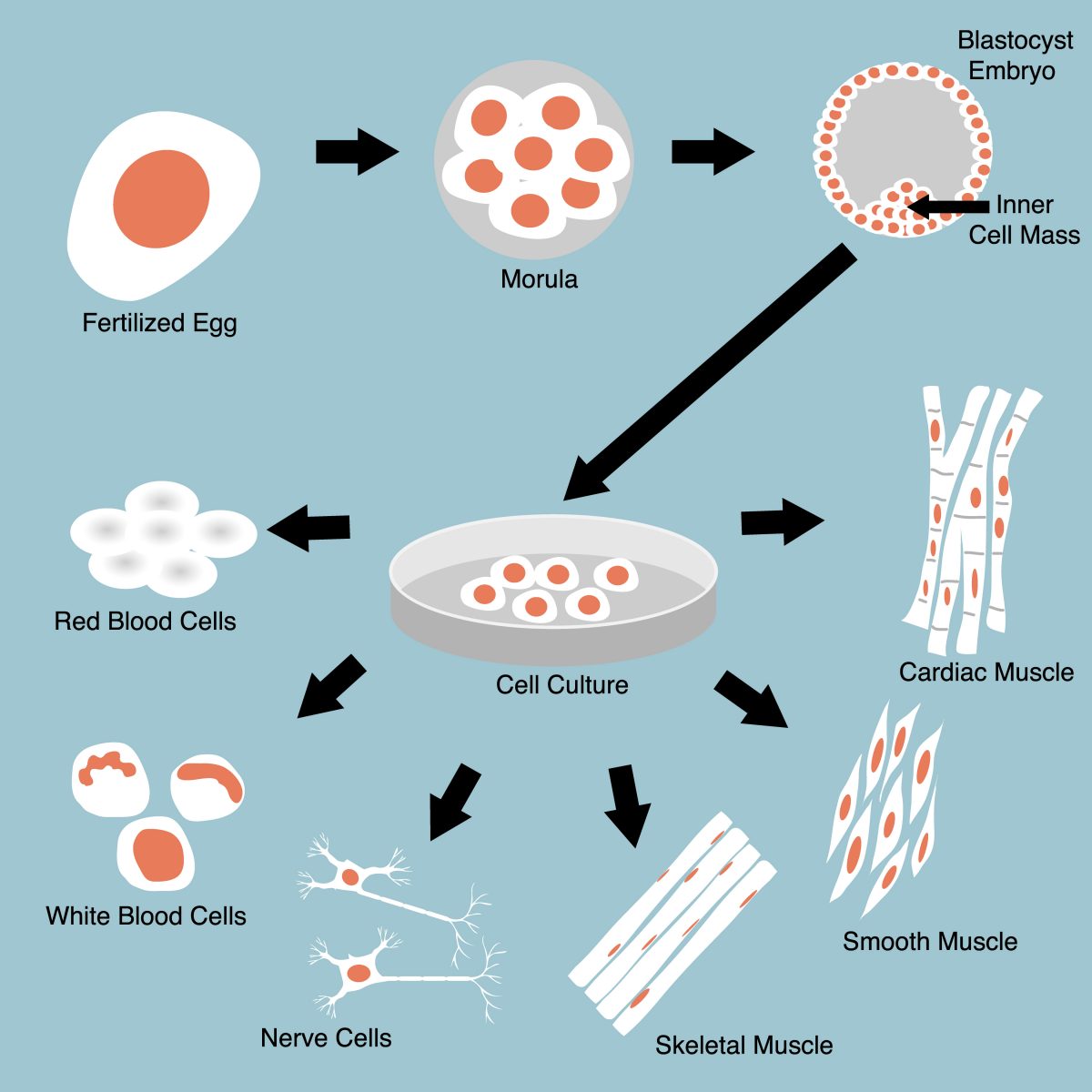
In this study, scientists at the Center for iPS Cell Research and Application (CiRA), Kyoto University in collaboration with colleagues at the Institute for Frontier Medical Sciences, Kyoto University established an in vitro model to screen for drugs with therapeutic value for DMD and investigate the molecular basis for the disease using human induced pluripotent stem cells (hiPSCs). Scientists extracted (by biopsy) skin fibroblasts from 2 different patients diagnosed with DMD, and reprogrammed these fibroblasts back into pluripotent stem cells, using a well-established method for generating hiPSCs. The team then introduced a gene that differentiates iPS cells into muscle cells, thus allowing them “to use the same genetic background to study the early stage of pathogenesis which was not possible in the past,” noted CiRA researcher Emi Shoji and the study’s first author.
With this in vitro system, scientists could now recapitulate the early pathogenesis of DMD and study its causes while screening for new drugs.
The initial trigger of muscle damage in DMD was suggested to be an excess of calcium ion (Ca2+) influx into skeletal muscle cells, accompanied by an increase in muscle cells’ plasma membrane injuries. As such, targeting these initial pathogenic events is considered a key strategy to develop DMD therapeutics, as Shoji noted, “It is critical to assess intact cells for an accurate evaluation how Ca2+ influx leads to DMD pathogenic cascades.”
Authors used their system and stimulated muscle cell contraction, by electric impulses, measuring Ca2+ influx. They observed that indeed DMD patients’ muscle cells had a significant increase in Ca2+ influx, and that this is one of the earliest events occurring in dystrophin-deficient muscle cells (in response to electric stimuli). They discovered the TRP channels – mechanically activated by Ca2+ and expressed in skeletal muscle cells – are responsible for this pathogenic Ca2+ influx.
This observation is in agreement with previous studies (reporting that Ca2+ influx induced muscular dystrophy in control muscle fibers through a TRP channel-dependent mechanism) and identified the TRP- Ca2+ pathway as a potential effective drug target for DMD therapeutics.
Hidetoshi Sakurai, study corresponding author commented on the clinical potential of their findings, “TRP channels have been identified before. But because our model uses patient-derived hiPS cells, there is a potential that we can find new drugs for DMD.”