Preimplantation Genetic Screening Procedures May Reduce Genetic Diseases
 One of the largest networks of fertility experts in California, Advanced Reproductive Care (ARC) Fertility, is advocating for the performance of new preimplantation genetic diagnosis (PGD) techniques and preimplantation genetic screening (PGS). The physicians within the network believe the procedures can help more families successfully benefit from fertility treatments and reduce the probability of their unborn child developing debilitating conditions such as muscular dystrophy.
One of the largest networks of fertility experts in California, Advanced Reproductive Care (ARC) Fertility, is advocating for the performance of new preimplantation genetic diagnosis (PGD) techniques and preimplantation genetic screening (PGS). The physicians within the network believe the procedures can help more families successfully benefit from fertility treatments and reduce the probability of their unborn child developing debilitating conditions such as muscular dystrophy.
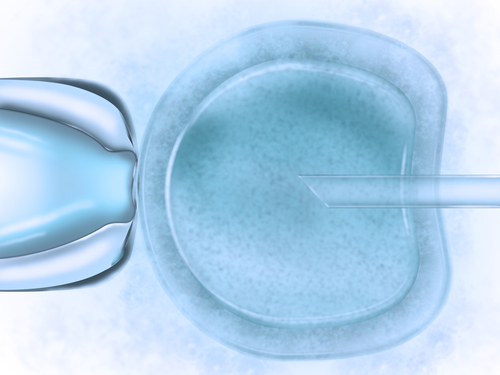
Both PGD and PGS are among the novel developments currently focused on by numerous reproductive and fertility scientists, embryologists and physicians who seek to provide families healthier pregnancies and children. According to ARC Fertility, the two procedures can be helpful additions to fertility treatments in order to improve the likelihood of carrying healthy babies.
“PGD has contributed to the reduction of debilitating genetic disorders such as cystic fibrosis, Huntington’s Disease, muscular dystrophy, and many others,” said the founder and CEO of ARC, David Adamson, in a press release. “PGS is a new technology that is being used to select the healthiest embryos prior to implantation. It has been shown to reduce the risk of miscarriage and results in higher implantation rates. Its optimal role in managing IVF patients is still being evaluated. Both PGD and PGS, when used appropriately in selected patients, can play an important role in healthy pregnancies and healthy children.”
[adrotate group=”3″]
PGD can be conducted on the day 5 embryo (blastocyst), to search for determined genetic abnormalities. ARC Fertility advocates its use particularly in couples determined to be at high risk of having children with genetic disorders, such as muscular dystrophy. In addition, the network explained that recent estimations calculated the global preimplantation genetic diagnosis market as an expansionary one, set to reach $47.4 million by the end of 2018.
PGS, on the other hand, which is still being studied in clinical trials to understand its optimal performance, is indicated for infertile couples or patients who recurrently lose their fetuses. The procedure is based on the screening of a blastocyst to determine the normality of the chromosomes, which may help physicians determine the most normal blastocysts for transfer into the uterus.
“PGD and PGS are technologies that can only be performed because IVF, which creates embryos in the laboratory, was developed,” added Adamson. “Screening gives us the ability to test those embryos before implantation and avoid implanting an embryo that has an abnormality. It allows us to give our patients peace of mind in an already stressful and complicated situation.”