Study Traces Molecular Pathway Leading to Muscle Regeneration
Written by |
University of Louisville researchers have discovered that a mechanism involved in stem-cell renewal pathways and muscle tissue regeneration, with implications in muscular dystrophy research. The study, titled “TRAF6 regulates satellite stem cell self-renewal and function during regenerative myogenesis,” was published in the Journal of Clinical Investigation.
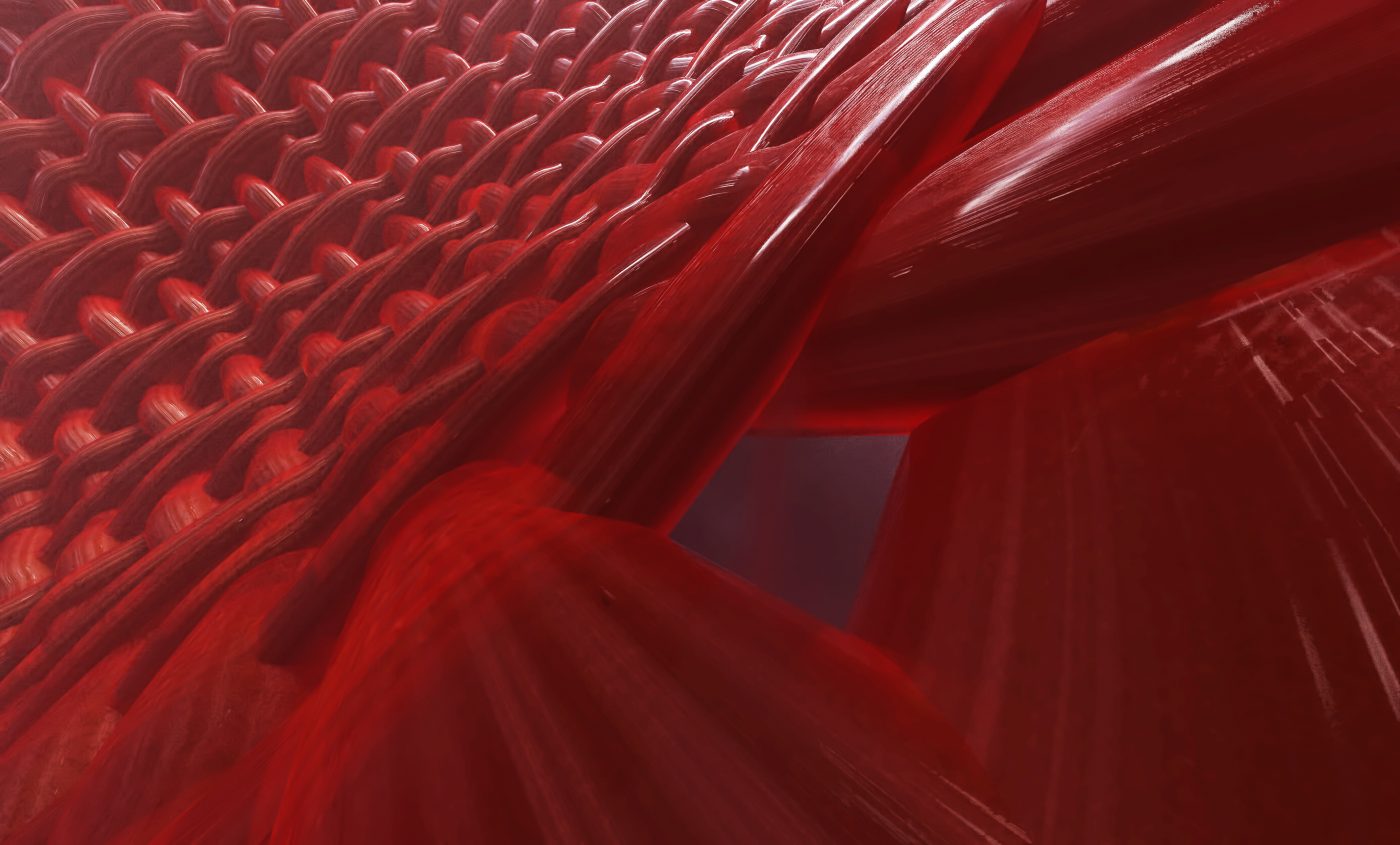
In muscle injury a cascade of signals is triggered to activate satellite cells, a dormant stem cell population in adult muscle tissue that allows new muscle fibers to be generated. While a great portion of these cells turn into muscle cells, a small portion undergo self-renewal and return to a dormant state to prepare for future injury.
Previous research has demonstrated that muscle regeneration and satellite cell self-renewal are dependent on the transcription factor Pax7. When this crucial protein is decreased or not present, satellite cells undergo permanent and premature differentiation and lose their self-renewal abilities, hindering their capacity to regenerate damaged muscles. The molecular mechanisms behind the regulation of Pax7 levels and this self-renewal process, however, are still poorly understood.
Study authors, Drs. Sajedah M. Hindi and Ashok Kumar, discovered that TNF receptor-associated factor 6 (TRAF6) is essential for Pax7’s role and maintenance. Using healthy and Duchenne muscular dystrophy (DMD) mice, researchers observed that removal of TRAF6 led to the depletion of Pax7 and to reduced muscle regeneration in both models. “We have discovered a pathway by which the Pax7 and myogenic potential of satellite cells is regulated. The protein TRAF6 is a very important adaptor protein that is involved in multiple signaling pathways and its functions are important to maintain the stemness of satellite cells in adults,” Dr. Kumar said in a press release.
The researchers further explained that in disease states, such as muscular dystrophies, satellite cells are exhausted from the level of regeneration demanded by repeat cycles of injury and tend to become functionally impaired. In the future, the team intends to investigate if this impairment is due to lack of TRAF6 signaling and, if confirmed, whether restoring TRAF6 activity in patients’ own satellite cells could constitute a new therapy approach. As Dr. Kumar explained, “Right now, the problem in donor stem cell therapy is that we inject the stem cells into the patient but most of the stem cells don’t proliferate very well, so they repair very little part of the muscle. But if you have stem cells that are over-expressing this protein TRAF6, they may proliferate longer and they may repair the muscle much more effectively.”