Muscular dystrophy overview
Last updated Sept. 11, 2025, by Lindsey Shapiro, PhD

Muscular dystrophy (MD) refers to a group of rare genetic muscle disorders characterized by progressive muscle weakness and wasting.
Each type of MD has its own clinical profile and prognosis, with some emerging early and progressing quickly and others showing up later in life and progressing slowly.
There is no cure for MD, but a prompt diagnosis and early treatment initiation can help manage symptoms, prevent complications, and in some cases, slow the disease’s progression.
What is muscular dystrophy?
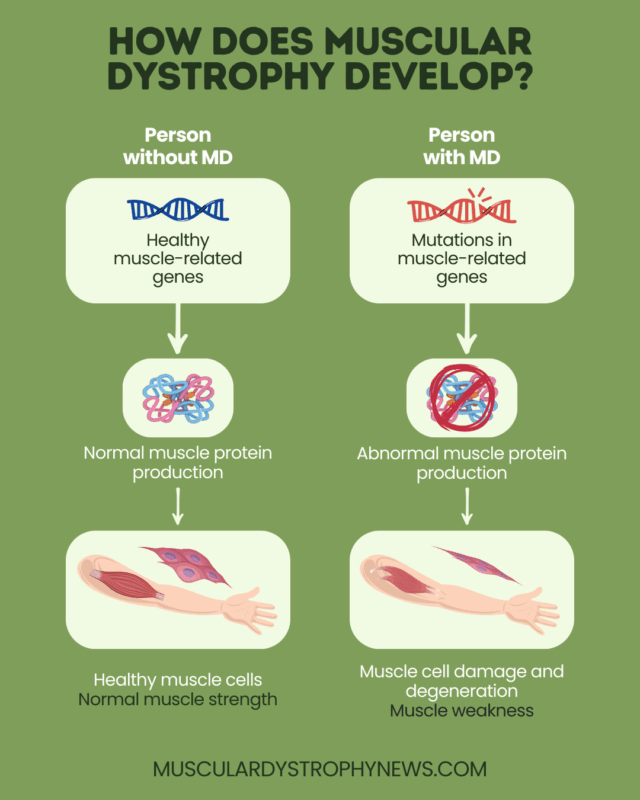
MD encompasses a large group of disorders characterized by muscle degeneration and weakness due to genetic mutations that affect muscle health. The skeletal muscles that control voluntary movements are most typically affected, but other muscles — like those needed for the heart to beat — may also be impacted.
As a progressive disease, the symptoms of MD tend to get worse over time, although the rate at which this happens varies substantially. In some cases, MD is evident in infancy or childhood and progresses rapidly to complete functional disability, while in others, mild muscle weakness doesn’t appear until adulthood and never leads to a complete functional loss.
MD is considered relatively rare, affecting an estimated 1 in every 5,000-10,000 people worldwide. However, the clinical diversity of MD can make it challenging to accurately estimate its true prevalence. Duchenne MD (DMD) — the most common form of the disease – is thought to affect around 1 in 3,500 male births globally.
Muscular dystrophy causes
MD is caused by genetic mutations that negatively affect muscle health. Each form of MD is caused by problems in different genes, but they all ultimately result in muscle weakness.
For example, DMD and its milder counterpart Becker MD (BMD) are caused by mutations in the DMD gene that result in no or low dystrophin, a protein that’s important for protecting muscles against damage.
In most cases, MD-causing mutations are passed down in families when children inherit them from their parents. The exact pattern of inheritance varies, with some forms, like DMD and BMD, being seen mainly in males, while others affect the sexes equally. Less frequently, disease-causing mutations can arise spontaneously in a person without a family history.
Muscular dystrophy types
There are more than 30 different types of MD, all with their own underlying genetic MD causes, symptoms, progression, and treatments.
The most common are DMD and BMD, with DMD being a severe form that emerges in childhood and progresses quickly to a complete loss of physical function. BMD, on the other hand, more commonly emerges in adolescence and takes a milder course.
Other MD types include:
- Myotonic dystrophy, the most common adult-onset form of MD
- Facioscapulohumeral MD (FSHD), which mainly affects muscles in the face, shoulders, and upper arms
- Limb-girdle muscular dystrophy (LGMD), characterized mainly by weakness in muscles around the shoulders and hips
- Congenital muscular dystrophy [kw] (CMD), a group of conditions where muscle weakness is evident at birth or in infancy
- Emery-Dreifuss muscular dystrophy (EDMD), characterized by weakness in the shoulders, upper arms, and lower legs
- Distal muscular dystrophy, affecting muscles farther from the core of the body
- Oculopharyngeal muscular dystrophy (OPMD), where weakness mainly affects the eyelids and throat
Beyond muscle weakness and movement problems, each MD type may come with a variety of other symptoms. Knowing the specific disease type is key to proper treatment and care.
Muscular dystrophy symptoms
The hallmark of MD is progressive muscle weakness and atrophy. The specific symptoms that result from this depend on which muscles are affected, but could include:
- delayed motor milestones, like sitting up, crawling, or walking
- frequent falls and clumsiness
- difficulty rising from a sitting or lying down position
- waddling gait
- walking on the toes
- trouble using the arms or hands for reaching, lifting, or gripping
- muscle and joint pain or stiffness
- enlarged calf muscles
Various other MD symptoms are also possible, depending on the specific disease type and severity. These could include:
- scoliosis, a sideways curvature of the spine
- contractures, where muscles and tendons become short and inflexible, leading to joint stiffness
- cognitive problems
- fatigue
- breathing difficulties
- heart disease
- eye problems
- speech and swallowing difficulties
Muscular dystrophy diagnosis
Diagnosing MD usually starts with a clinical evaluation, including a review of family and personal medical history, as well as a physical exam. If MD is suspected, a variety of other diagnostic tests may be done to confirm a MD diagnosis and establish the disease type. These may include:
- genetic testing, to identify a disease-causing mutation and rule out another inherited muscle disorder
- blood tests, to measure markers of muscle damage
- electromyography, to assess the health of muscles and the nerves that control them
- imaging studies, such as a MRI scan, to visualize muscles and look for hallmarks of MD
- muscle biopsy, to look for cellular changes consistent with MD in a muscle tissue sample
- six-minute walk test, which evaluates physical function
Physicians will use these tests to look for signs of MD and rule out any other neuromuscular disorder that could have overlapping symptoms. Nowadays, genetic testing is the most definitive way to establish MD and hone in on which disease type is present.
Muscular dystrophy treatment
Although there is no cure, an appropriate multidisciplinary MD care plan can help ease symptoms and make living with MD easier.
Most forms of MD are treated with supportive care approaches that are intended to help preserve function, prevent complications, and make daily life easier.
Medications vary, based on a person’s specific symptoms, but may be intended to preserve heart function, ease gastrointestinal symptoms, or support bone health. These may be used along with non-drug interventions such as:
- physical therapy, to improve muscle strength and mobility
- occupational therapy, to make activities of daily living easier
- speech therapy, to ease speech and swallowing issues
- ventilation, or other interventions to support breathing
- surgery, to address complications like scoliosis or contractures
There are also a number of approved medications for people with DMD that may be able to preserve muscle strength and slow disease progression, including:
- oral corticosteroids, such as prednisone, Emflaza (deflazacort), and Agamree (vamorolone)
- exon-skipping therapies, given via infusions into the bloodstream, including Amondys 45 (casimersen), Exondys 51 (eteplirsen), Viltepso (viltolarsen), and Vyondys 53 (golodirsen)
- gene therapy, given as a one-time infusion, including Elevidys (delandistrogene moxeparvovec-rokl)
- Duvyzat (givinostat), an oral histone deacetylase (HDAC) inhibitor
Ongoing research is focused on developing new disease-modifying therapies, including gene therapies, for DMD and less common forms of the disease.
Muscular dystrophy life expectancy
MD life expectancy varies substantially, depending on factors that include disease type, complications, and disease management.
Until recently, boys with DMD did not usually survive past adolescence. But with improvements in MD treatment and care, many with DMD are surviving into their 20s or 30s. Most people with BMD live well into middle or late adulthood, and can have a normal or near normal lifespan.
Other forms of MD are more variable, but most people with FSHD, OPMD, EDMD, and distal MD have a relatively normal lifespan with proper disease management. The MD prognosis for other types, such as myotonic MD, LGMD, and CMD highly depends on the disease subtype.
For any type of MD, a prompt diagnosis and an early start to multidisciplinary treatment is key for ensuring the best possible long-term outcomes and quality of life. As newer disease-modifying therapies emerge, the outlook for MD could change in years to come.
Muscular Dystrophy News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- I have new criteria for when my sons participate in DMD clinical trials
- New gene therapy for OPMD shows lasting success in small US trial
- How art fosters a sense of belonging in my life with Duchenne
- First boys dosed in Phase 2 trial of oral DMD treatment SAT-3247
- Guest Voice: Despite losses from Duchenne MD, I persevere