Ataluren for Duchenne muscular dystrophy
Last updated May 22, 2024, by Marisa Wexler, MS

What is ataluren for Duchenne muscular dystrophy?
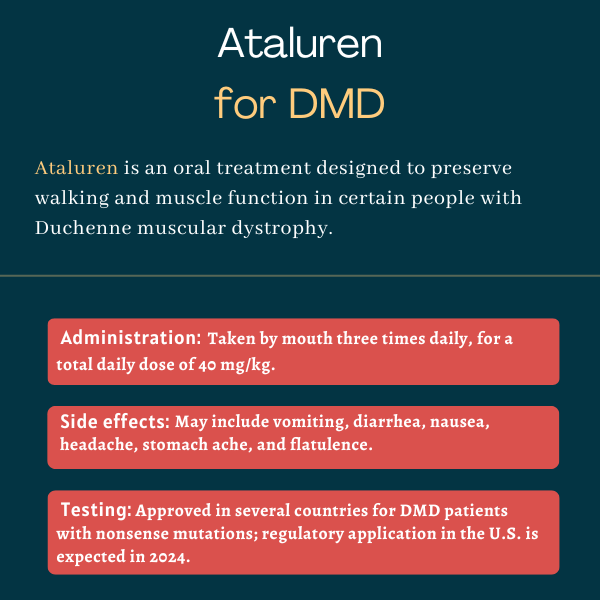
Ataluren is an oral small molecule designed to preserve walking and muscle function in people with Duchenne muscular dystrophy (DMD) caused by so-called nonsense mutations.
The therapy, developed by PTC Therapeutics, was conditionally approved in the European Union (EU) in 2014, under the band name Translarna, and can treat patients ages 2 and older who retain the ability to walk. But a committee at the European Medicines Agency recommended against renewing the conditional approval early in 2024, meaning the medication is to be withdrawn from the market.
In the U.S., an initial application seeking ataluren’s approval was rejected in 2017 by the U.S. Food and Drug Administration (FDA), which said there wasn’t enough evidence to support its effectiveness in DMD. However, based on agency feedback, PTC announced it was planning to resubmit an application by mid-2024.
The medication currently is approved in several other countries, in addition to those in Europe.
Therapy snapshot
| Treatment name: | Ataluren |
| Administration: | Tested in Duchenne muscular dystrophy as oral granules |
| Clinical testing: | Phase 3 trial completed; approved in several countries outside the U.S. |
How does ataluren work?
DMD is a progressive condition characterized by gradual muscle weakening. The disease is caused by mutations in the DMD gene, which codes for a protein called dystrophin that is essential for protecting muscles from damage during movement.
Symptoms of DMD can begin as early as age 2. As the disease progresses, patients find activities such as walking increasingly difficult, and may develop scoliosis (a sideways curvature of the spine), as well as digestive, respiratory, and cardiac problems.
Ataluren is designed to treat patients who carry a particular DMD gene defect called a nonsense mutation. This type of mutation introduces a stop signal in the gene, prematurely halting the synthesis of the dystrophin protein.
The result is a smaller, truncated protein that cannot function normally and is rapidly destroyed by the cell. Up to 15% of DMD cases are caused by a nonsense mutation.
Ataluren forces the cell to ignore this abnormal stop signal, enabling the production of a full-length, functional protein. Thus, it works as a “protein restoration therapy,” which means that it aims to facilitate the production of a functional protein in patients who cannot produce it normally.
How will ataluren be administered in DMD?
In DMD clinical trials, ataluren was administered to patients as oral granules that were mixed with a liquid or soft food (e.g., yogurt, apple sauce). It was mainly tested at doses ranging from 10 to 80 mg per kilogram of body weight.
In Europe, the therapy is administered in three daily doses — a 10 mg/kg dose in the morning and at midday, and a 20 mg/kg dose in the evening — for a total daily dose of 40 mg/kg. Doses should be taken at least six hours apart.
It’s not known if these will be the recommended dose and dosing schedule should the therapy be approved in the U.S.
Ataluren in clinical trials
Ataluren’s safety and efficacy have been studied in two randomized clinical trials: a Phase 2b study (NCT00592553) that enrolled 174 patients and a Phase 3 trial (NCT03179631) involving 360 participants.
Both enrolled boys and men ages 5 and older who carried nonsense mutations in the DMD gene, and randomly assigned them to either ataluren or a placebo. These trials formed the basis for the therapy’s approval in Europe.
Phase 2b trial
The Phase 2b study tested the 40 mg/kg dosing regimen (given as 10 mg/kg in the morning, 10 mg/kg at midday, and 20 mg/kg in the evening) and a higher dose of 80 mg/kg per day against a placebo.
Participants, ages 5-20, had elevated levels of creatine kinase, a marker of muscle damage, but were able to walk unassisted at least 75 meters (246 feet) during the six-minute walking test (6MWT), a standard measure of functional capacity.
The trial’s main goal was to determine whether either tested dose could increase the distance walked in six minutes after 48 weeks of treatment compared with a placebo. Secondary assessments included other timed function tests, such as the 10-meter run/walk test, the four-stair climbing test, and the ability to stand when lying on the back or with the face upward, as well as changes in joint extension, falls, and quality of life.
Results showed that the treatment was generally well tolerated and significantly slowed the worsening in walking function compared with a placebo. After 48 weeks, 44% of patients on a placebo experienced a 10% or greater worsening in 6MWD, compared with 26% of those given the 40 mg/kg dose — corresponding to a 48% reduction in the risk of worsening.
The greatest benefits were observed in patients who were already losing their ability to walk. In turn, patients given the higher dose behaved similarly to the placebo group.
Clinically meaningful benefits with the 40 mg/kg daily dose likewise were found in other timed function tests, where patients given ataluren experienced smaller increases in the time taken to perform those tests than patients on a placebo. The frequency of falls also fell significantly with ataluren, and there was a trend toward a better physical quality of life.
Phase 3 trial
The international Phase 3 trial, called Study 041, enrolled participants who could walk at least 150 meters during the 6MWT and randomly assigned them to the 40 mg/kg regimen or a placebo for 72 weeks (about 1.5 years).
This study aimed to demonstrate that ataluren would lead to 6MWD improvements as in the previous trial. Secondary goals also were similar to the Phase 2 study.
Results generally showed that participants given ataluren experienced a 21% slower decline on 6MWD compared with those given a placebo after 72 weeks. Also, fewer patients on ataluren lost the ability to walk, and the time to a 10% decrease in 6MWD was significantly longer for treated patients.
Treatment benefits again were greatest in a group of patients with poorer walking function — walking between 300 to 400 meters on the 6MWD — whose decline in 6MWD was reduced by 30% with ataluren. Ataluren treatment was well tolerated, with no serious adverse events thought to be related to the therapy.
STRIDE registry
An ongoing observational global study (NCT02369731) called STRIDE (Strategic Targeting of Registries and International Database of Excellence) is following patients using ataluren in countries where the therapy is approved. Participants are receiving ataluren plus standard DMD care (including corticosteroids) and being followed for at least five years.
Data covering 268 patients in this registry showed that ataluren delayed the loss of walking abilities by four years, compared with a control group of patients given standard treatment alone.
In treated patients, lung function also declined more slowly than in the control group, reaching a point where respiratory physical therapy was needed about 1.8 years later. The treatment has been well tolerated, with adverse events consistent with the medication’s known safety profile.
Common side effects of ataluren
The most common side effects of ataluren include:
- vomiting
- diarrhea
- nausea
- headache
- stomach ache
- flatulence.
Muscular Dystrophy News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- New research reveals protein pathway that can slow muscle repair
- Dreaming of solutions to the Olympic-sized challenges of FSHD
- Roche halts development of satralizumab for DMD bone health
- An essay on choosing hope in life with a progressive, degenerative disease
- I have new criteria for when my sons participate in DMD clinical trials
Related articles




